Best Cosmetic & Plastic Surgeons in Indraprastha Apollo Hospital Delhi
 29 January,2026
Read More
29 January,2026
Read More
Enquire now in case of any assistance needed

Immunotherapy, a word that has gained popularity in recent years, has been used longer than you imagined. In 1891, William B. Coley pioneered one of the earliest forms of immunotherapy by injecting streptococcal bacteria into a cancer patient, successfully shrinking the tumor. Over the next four decades, he treated over 1,000 patients with bacterial products known as Coley's Toxins, reporting significant success, especially in sarcomas. Despite his promising results, skepticism from the medical community and the rise of radiation and chemotherapy led to the decline of his methods. Today, Coley is recognized as the "Father of Immunotherapy," with modern science validating his groundbreaking idea that enhancing the immune system can combat cancer.
This blog explores immunotherapy in detail, from the cancers it treats to its benefits and risks. Let's learn more about the latest advancements in immunotherapy and whether it's right for you.
Fill up the form and get assured assitance within 24 hrs!
Immunotherapy is an FDA-approved cancer treatment that helps the immune system fight cancer. The immune system is your body's defense system, made up of white blood cells (WBCs), tissues, and organs that work together to protect you from infections and diseases. It can also help protect you from cancer. The immune system works by identifying substances in your body. If something doesn't belong, like germs or cancer cells, it sees them as "foreign" and attacks them. However, cancer cells are tricky because they start as normal cells that change and grow out of control. This makes it hard for the immune system to always recognize them as a threat.
Sometimes, the immune system doesn't attack cancer because the cells look too much like normal ones. Other times, the immune system tries but isn't strong enough, or the cancer cells produce substances to block the attack. Immunotherapy helps by giving the immune system extra support to recognize and attack cancer cells more effectively. It's a type of treatment that uses living substances to help the body fight cancer on its own.
Immunotherapy can be delivered in different ways depending on the type of drug and the patient's needs. Here's how it is typically given:
Intravenous and Injection Procedures
If immunotherapy is delivered into a vein, it can be done through:
Treatment Process for Administering Immunotherapy
Patients often visit a clinic or day unit as outpatients. Depending on the medication, drugs may be given via pump, with the dose controlled over 10 minutes to several hours. The nurse will guide patients through the treatment schedule and procedure for each session.

There are different types of immunotherapies. They target cancer by stimulating the immune system or enhancing its ability to recognize and attack cancer cells. Each immunotherapy type has specific mechanisms and applications depending on the cancer being treated.
Checkpoint inhibitors are drugs designed to interfere with the immune system's natural "off switches," which cancer cells often exploit to avoid detection.
Adoptive cell therapy is a personalized immunotherapy approach in which a patient's immune cells are collected and modified in a laboratory. They are then reintroduced into the body to target cancer better. The two main types are:
Emerging ACT technologies include CAR natural killer (NK) cell therapy, which utilizes NK cells from sources like umbilical cord blood and enhances their ability to detect and destroy cancer cells. Endogenous T cell (ETC) therapy involves selecting and expanding specific cancer-fighting T cells from a patient's blood.
Monoclonal antibodies are laboratory-made proteins designed to bind to specific targets on cancer cells or within the tumor environment. These therapies work in several ways:
Radioimmunotherapy, like ibritumomab, uses monoclonal antibodies linked to radioactive substances to deliver targeted radiation to cancer cells. Monoclonal antibody therapies are commonly used for cancers like breast cancer, colorectal cancer, and lymphoma.
Cancer vaccines activate the immune system to recognize and fight cancer cells. Preventive vaccines, such as those for human papillomavirus (HPV) and hepatitis B virus (HBV), reduce the risk of virus-associated cancers like cervical and liver cancer. Therapeutic cancer vaccines, like sipuleucel-T for prostate cancer, are designed to activate the immune system against existing cancer. These vaccines often use tumor-specific antigens, sometimes sourced directly from the patient's cancer, to train the immune system to target the tumor more effectively.
Immune system modulators are therapies that enhance the general activity of the immune system rather than targeting cancer cells directly. Key examples include:
These therapies include agents that enhance the immune system's overall capacity to fight cancer. Examples include toll-like receptor agonists (which stimulate immune cells to recognize and attack tumors) and granulocyte-macrophage colony-stimulating factors (which encourage the production of white blood cells that help combat cancer and infections).
Common cancers treated with different types of immunotherapies are:
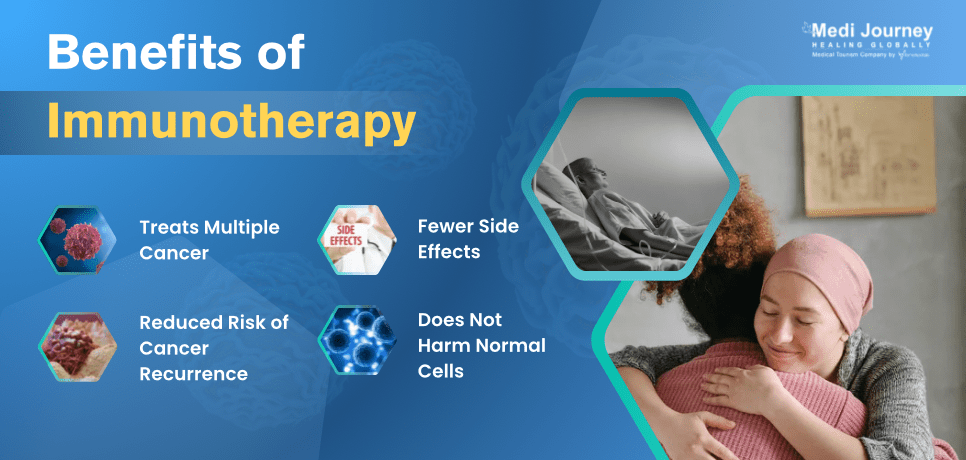
Immunotherapy offers numerous benefits that make it a compelling option for cancer treatment. These benefits address the challenges posed by traditional therapies, enhance treatment outcomes, and improve the quality of life for many patients. Here's an in-depth look at the advantages:
Immunotherapy, while promising as a treatment for cancer and certain autoimmune diseases, comes with potential side effects ranging from mild to severe. Understanding these effects is essential for patients and healthcare providers to manage treatment effectively. Here are some common side effects of immunotherapy:
Immunotherapy strengthens the immune system to target disease-causing cells. However, this supercharged response may mistakenly attack healthy cells, resulting in side effects. While most of the side effects are mild and manageable, the risk of severe complications necessitates careful monitoring during treatment.
Immunotherapy is a cancer treatment that helps your body's immune system fight cancer cells. It works in different ways, like teaching your immune system to recognize cancer cells better or blocking signals that help cancer cells hide. Immunotherapy has very few side effects compared to other treatments like chemotherapy and can even work when other treatments have stopped helping. While immunotherapy isn't right for everyone, it's a promising new approach that's giving many people with cancer hope for better outcomes.
Fill up the form and get assured assitance within 24 hrs!
Doctor of Pharmacy
Dr. Deepanshu Siwach is a skilled clinical pharmacist with a Doctor of Pharmacy degree.?He has 4+?years of experience and has worked with thousands of patients. He has been associated with some of the top hospitals, such as Artemis Gurgaon.
Senior Director
Medical Oncologist
Dr. Sajjan Rajpurohit is a leading medical oncologist in New Delhi. With over 22 years of experience in cancer treatment, he has performed more than 15,000 immunotherapy cycles. His specializations include immunotherapy, targeted therapy, and chemotherapy for solid tumors (breast, lung, gastrointestinal, genitourinary, head and neck, and sarcoma)....
Yes, people with HIV can receive immunotherapy, but it requires careful evaluation. Since immunotherapy stimulates the immune system, patients with compromised immune function, like those with HIV, must be monitored closely. The decision to use immunotherapy depends on the individual's overall health, the type of cancer, and how well their HIV is managed.
Immunotherapy helps the immune system learn to recognize and remember cancer cells. This ability (immunomemory) can lead to long-lasting protection against cancer returning. Studies show that patients who respond well to cancer immunotherapy can have lasting benefits. These positive effects can continue even after finishing treatment.
The effectiveness of immunotherapy is typically assessed through regular imaging scans (like CT or PET scans) and blood tests to monitor tumor size and biomarker levels. Patients might also notice improvements in symptoms, such as reduced pain or better physical functioning. However, it's important to note that immunotherapy may take longer to show results compared to other treatments. In some cases, tumors may initially appear larger due to inflammation caused by the immune response.
Immunotherapy is suitable for many patients, but eligibility depends on factors like:
Patients with autoimmune diseases or organ transplants may not be ideal candidates due to the risk of exacerbating immune-related complications. Your oncologist can determine if immunotherapy is appropriate for your situation based on detailed medical evaluations and test results.
Senior Consultant
Medical Oncologist
Nanavati Super Specialty Hospital, Mumbai
WhatsApp UsSenior Director
Gynecologist and Obstetrician, IVF Specialist
Max Super Speciality Hospital, Shalimar Bagh, New Delhi
WhatsApp UsSenior Director
Gynecologist and Obstetrician, IVF Specialist
Max Smart Super Speciality Hospital, Saket, New Delhi
WhatsApp UsSenior Director
Gynecologist and Obstetrician
Max Smart Super Speciality Hospital, Saket, New Delhi
WhatsApp UsSenior Director
Gynecologist and Obstetrician
Max Smart Super Speciality Hospital, Saket, New Delhi
WhatsApp UsSenior Director
Gynecologist and Obstetrician
Max Smart Super Speciality Hospital, Saket, New Delhi
WhatsApp UsThe Art of Effective Communication
 27 January,2026
Read More
27 January,2026
Read More
 20 January,2026
Read More
20 January,2026
Read More
 16 January,2026
Read More
16 January,2026
Read More
 13 January,2026
Read More
13 January,2026
Read More
 09 January,2026
Read More
09 January,2026
Read More
Trusted by Patients
"I am Asim from Bangladesh and was looking for treatment in India for neuro. I visited many websites to get the complete information regarding the treatment but I was not satisfied as I was getting confused. In the meanwhile, one of my friends suggested I seek help from Medi Journey as he experienced his medical journey very smoothly and was satisfied with it. They have filtered the top 10 doctors as per experience, the success rate of surgery & profile, so it helps us to choose the best treatment in India. "
"For my knee surgery, Medi Journey guided me to BLK Hospital where I received exceptional care. The team's support and the expertise at BLK Hospital exceeded my expectations. Thank you Medi Journey for making my medical journey stress-free. "
"I came from Iraq for my granddaughter's eye surgery in India facilitated by Medi Journey, due to critical cases they advised us to get a second opinion from the different hospitals before going to surgery. Finally, we went to Fortis Escort Hospital, which helped us to get more confidence for diagnosis. Fortis Escort Hospital has the best eye surgeon team with the latest instruments. Thanks to all team members for providing a high-quality treatment in India at an affordable cost. "
"I came for my hair transplant in India, before coming I was so confused about choosing the best clinic and surgeon for me. But thanks to God one of my friends had a hair transplant in India through Medi Journey. He recommended me to go with them. I am completely happy with my experience with them. They were always very fast in their responses to me. the success rate of my hair transplant surgery is 100%."
"Artemis Hospital, suggested by Medi Journey, turned out to be a great choice for my treatment. The personalized assistance and medical care were exceptional. I'm grateful to Medi Journey for guiding me to a hospital that perfectly matched my needs. Highly recommended! "
"I came from Afghanistan for my treatment in India at Jaypee Hospital, Noida. I had a fantastic experience with Medi Journey. Kudos to them for their incredible support during my medical journey. They not only took care of all the logistics but also connected me with a fantastic healthcare team. Efficient, caring, and highly recommended for a hassle-free medical tourism experience."
"I am Adam from Kano, Nigeria, one of my friends from Nigeria was facilitated by Medi Journey, and he recommended us to go with them. I sent my all reports to them and within 48 hours they reverted with 4 options from different hospitals. They helped me to get a Visa letter from the hospital, arrange pick-up from the airport, and book a hotel for me. Their team is very honest and throughout our stay in India they are with us they are caring for us like his family members. BLK Hospital is the best hospital in India with a top surgical oncologist surgeon team, a very advanced OT, and a Radiotherapy department. I wish more success to Medi Journey. "
"Great experience at the Max Hospital for my spine surgery and was successfully done. I thank my neurosurgeon and his entire team. I recommended all of my country's people to Medi Journey for treatment in India, they choose the best hospital, the best doctors, and the best cost for patients."
"I came to India from Dhaka, Bangladesh for my father-in-law's cardiac surgery at Fortis Hospital. I was confused about choosing the best surgeon for him before coming, but their team helped me to choose the best hospital and best cardiac surgeon in India with very good cost and 100% success rate of surgery. I am very happy with the services, really they make my journey so comfortable that make me feel at home. Thanks again and I like people to choose "Medi Journey" as your travel guide. "
"I am Mohammad from Bangladesh came to India for my general health checkup. Medi Journey offers me the complete package including Pick-up from the airport, hotel services, and 24-hour assistance. They guide you to choose the best hospital in India, the best cost of treatment with top-most doctors and give you complete information about hotel booking, and pick-up from the airport before coming to India They have the best team to help. Always choose Medi Journey for your treatment in India."