Top Nephrologists in Indraprastha Apollo Hospital Delhi
 04 February,2026
Read More
04 February,2026
Read More
Enquire now in case of any assistance needed

We understand that getting diagnosed with pancreatic cancer can feel overwhelming and frightening. But remember, you are not alone in this journey. We are here to help you understand what this diagnosis means, what to expect, and the treatment options. This article covers everything you need to know about pancreatic cancer, including its symptoms, causes, risk factors, complications, and outcome.
Fill up the form and get assured assitance within 24 hrs!
Pancreatic cancer develops when cells in the pancreas grow out of control and form a tumor. The pancreas is a small, fish-shaped organ located behind your stomach. It plays a vital role in two main areas:
If cancer happens in the pancreas, it can disrupt these functions and cause a variety of symptoms.
Pancreatic cancer is categorized into two major types: exocrine pancreatic cancer, which accounts for over 95% of cases, and neuroendocrine pancreatic cancer, making up less than 5%.
Understanding the type of pancreatic cancer you have will help guide the treatment approach.
Pancreatic cancer statistics underscore the severity and challenges of this disease.
While these numbers may seem daunting, advancements in treatment and early detection are improving outcomes.
Pancreatic cancer is challenging to detect early because it often causes no noticeable symptoms in its initial stages. Additionally, its signs mimic many other illnesses. Symptoms often appear only after the cancer has spread. Here are the most common signs and symptoms:
These symptoms can also occur with other conditions, so it's essential to consult a doctor for proper evaluation.
Pancreatic cancer occurs when changes in DNA disrupt normal cell behavior. Healthy cells grow, multiply, and die in a controlled manner. Cancer cells, however, multiply rapidly and fail to die when they should. These cells can form a tumor that invades and damages healthy tissues. Over time, cancer cells may spread to other body parts.
The exact causes of mutations in the pancreatic cells are unclear, but certain factors increase the risk. Smoking and having a family history of pancreatic cancer are significant contributors. About 10% of cases are hereditary, meaning they result from inherited changes in DNA. However, most cases are caused by random mutations or external factors like obesity and aging.
If a first-degree relative has pancreatic cancer, your risk may be higher. Doctors recommend genetic testing for inherited mutations for affected family members. A negative test result often means no further testing is necessary. If results are positive or unclear, or if multiple family members have cancer, consulting a genetic counselor is advisable.
While the causes are not fully understood, early genetic testing and awareness of risk factors can help guide preventive strategies.
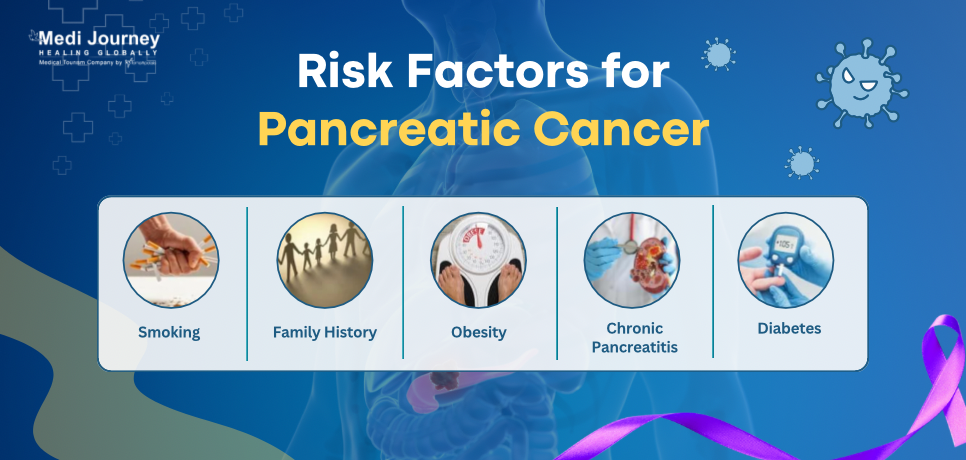
Some factors make certain people more likely to develop pancreatic cancer. These include:
Are you aware of any of these factors in your own history? Understanding these can help address specific risks.
Pancreatic cancer causes complications by affecting nearby structures, altering pancreatic function, or spreading to other areas. Some complications also occur due to the treatment.
By managing these complications proactively, doctors aim to improve treatment outcomes and quality of life, even in the advanced stages of pancreatic cancer.
Pancreatic cancer is challenging to detect early because the organ is placed deep in the abdomen, making it difficult to feel during routine exams. Additionally, small tumors are hard to see on standard imaging tests. If a doctor suspects pancreatic cancer, they may recommend a combination of tests, including imaging, blood tests, and genetic testing.
Doctors may recommend genetic testing if you are diagnosed with pancreatic cancer or have a family history of the disease. This testing identifies inherited gene mutations, such as BRCA1 and BRCA2, that increase the risk of pancreatic cancer and other cancers like breast, ovarian, or prostate cancer.
Why Consider Genetic Testing?
Even if you carry a mutation, it does not guarantee you will develop cancer, but knowing your risk is essential for early detection and management.

Pancreatic cancer is treated using a range of approaches that depend on factors such as the type and stage of cancer, its location, the overall health of the patient, and their personal preferences. Treatments aim to remove the cancer, slow its growth, reduce signs, and improve quality of life. Options include surgery, chemotherapy, radiation therapy, targeted therapy, immunotherapy, and palliative care, often used alone or in combination.
Surgical removal offers the potential for a cure in cases where the cancer is confined to the pancreas and can be completely removed. These are three main types of pancreatic cancer surgery:
Surgery can also be palliative, aiming to relieve symptoms rather than cure the disease. For example:
Chemotherapy utilizes medications to kill cancer cells or stop their growth. Chemo can be administered intravenously or in pill form. It is often used in cycles, allowing the body to recover between treatments. Chemotherapy is usually the primary treatment for advanced cancer, used before surgery to shrink tumors or given after surgery to kill any remaining cancerous cells. Common chemotherapy drugs for pancreatic cancer include capecitabine, gemcitabine, fluorouracil (5-FU), irinotecan, oxaliplatin, and their combinations. Side effects of chemo vary but may include nausea, vomiting, hair loss, and fatigue.
Radiation therapy employs high-energy X-rays or protons to target and kill cancer cells. This therapy can shrink tumors, make surgery possible, or relieve symptoms when surgery isn't an option. Treatments typically occur over several weeks, five days per week. Radiation may be combined with chemotherapy (chemoradiation) to enhance effectiveness. Side effects might include skin irritation, gastrointestinal issues, and fatigue, which usually improve after completing therapy.
Targeted therapy uses drugs to attack specific molecules or proteins that drive cancer cell growth. Examples include erlotinib (an EGFR inhibitor) and PARP inhibitors like olaparib. Because they focus on cancer-specific pathways, targeted therapies generally have fewer systemic side effects than chemotherapy. They may be combined with other treatments for greater effectiveness.
Immunotherapy enhances the immune system's ability to identify and destroy cancer cells. It is particularly effective in tumors with certain genetic alterations that make them more visible to immune cells. PD-1 inhibitors, such as pembrolizumab, are an example of immunotherapy drugs used for pancreatic cancer. Treatment is administered as an infusion every two to three weeks. Side effects might include fatigue, skin rashes, and joint pain.
Palliative care is an integral part of pancreatic cancer treatment, focusing on relieving symptoms and improving quality of life. It may involve managing pain (through medications, nerve blocks, or injections) and alleviating digestive issues caused by blockages in the bile duct or small intestine. Palliative radiation or surgery can reduce pain and complications caused by tumors. Additionally, psychological and emotional support is provided to address the mental health challenges associated with cancer.
Clinical trials give pancreatic cancer patients access to new and innovative treatments that are not yet available. These may include experimental drugs, new combinations of existing treatments, or advanced surgical techniques. Participation in a trial can provide hope, but patients should weigh potential risks and benefits with their care team.
Pancreatic cancer often causes significant pain, especially if it involves nearby nerves. Pain relief options include oral medications, anesthetic or steroid injections, and nerve blocks. These interventions help improve quality of life and enable patients to tolerate other treatments better.
Every case of pancreatic cancer is unique, and individual outcomes vary depending on the cancer's stage at diagnosis, treatment options, overall health, and response to therapy. While it's impossible to predict an exact prognosis for any individual, population-wide studies provide valuable insight into survival rates.
Survival rates for pancreatic cancer depend on the stage of the disease at the time of diagnosis:
For patients with stage IV pancreatic cancer, exploring all available treatment options, including clinical trials, is critical.
Surgery is one of the most effective interventions for pancreatic cancer when diagnosed early enough to allow tumor resection. For patients with tumors detected at the earliest stage (Stage IA), the five-year survival rate can exceed 80%, highlighting the importance of early detection.
Diagnosing pancreatic cancer at an operable stage can improve survival by more than tenfold compared to advanced-stage cases. Surgical candidates often undergo additional therapies, such as chemotherapy or radiation, to reduce recurrence risk and improve outcomes.
While current survival rates reflect historical data, advancements in treatment are improving outcomes for many patients. New therapies, including targeted treatments, immunotherapies, and participation in clinical trials, provide opportunities for better survival and quality of life. Continued research, early detection initiatives, and personalized treatment approaches offer hope for a brighter future in combating pancreatic cancer.
Pancreatic cancer continues to be a serious health challenge, but advancements in diagnostic techniques, surgical procedures, and treatments provide hope for improved survival and quality of life. Although the journey with this disease can be demanding, it's important to remember that you are not alone. Support groups, counseling, and friends and family can offer invaluable assistance during this difficult time.
Fill up the form and get assured assitance within 24 hrs!
Doctor of Pharmacy
Dr. Deepanshu Siwach is a skilled clinical pharmacist with a Doctor of Pharmacy degree.?He has 4+?years of experience and has worked with thousands of patients. He has been associated with some of the top hospitals, such as Artemis Gurgaon.
Senior Director
Medical Oncologist
Dr. Sajjan Rajpurohit is a leading medical oncologist in New Delhi. With over 22 years of experience in cancer treatment, he has performed more than 15,000 immunotherapy cycles. His specializations include immunotherapy, targeted therapy, and chemotherapy for solid tumors (breast, lung, gastrointestinal, genitourinary, head and neck, and sarcoma)....
Pancreatic cancer is curable only in early-stage cases that can be treated with surgery. Total surgical removal of the tumor is a way of curing prostate cancer.
Quitting drinking and smoking, eating a healthy diet, regular screenings, maintaining body weight, and staying active can reduce the risk of pancreatic cancer.
Treatment duration for pancreatic cancer depends on the stage and chosen therapies. It can range from weeks for surgery recovery to months for chemotherapy or radiation.
Clinical trials provide pancreatic cancer patients access to innovative treatments, including experimental drugs and new surgical techniques.
Getting diagnosed with pancreatic cancer can take a significant toll on mental health. Support groups, counseling, and stress-management techniques can help patients cope emotionally.
Senior Consultant
Medical Oncologist
Nanavati Super Specialty Hospital, Mumbai
WhatsApp UsSenior Director
Gynecologist and Obstetrician, IVF Specialist
Max Super Speciality Hospital, Shalimar Bagh, New Delhi
WhatsApp UsSenior Director
Gynecologist and Obstetrician, IVF Specialist
Max Smart Super Speciality Hospital, Saket, New Delhi
WhatsApp UsSenior Director
Gynecologist and Obstetrician
Max Smart Super Speciality Hospital, Saket, New Delhi
WhatsApp UsSenior Director
Gynecologist and Obstetrician
Max Smart Super Speciality Hospital, Saket, New Delhi
WhatsApp UsSenior Director
Gynecologist and Obstetrician
Max Smart Super Speciality Hospital, Saket, New Delhi
WhatsApp UsThe Art of Effective Communication
 04 February,2026
Read More
04 February,2026
Read More
 02 February,2026
Read More
02 February,2026
Read More
 27 January,2026
Read More
27 January,2026
Read More
 20 January,2026
Read More
20 January,2026
Read More
 16 January,2026
Read More
16 January,2026
Read More
Trusted by Patients
"I am Asim from Bangladesh and was looking for treatment in India for neuro. I visited many websites to get the complete information regarding the treatment but I was not satisfied as I was getting confused. In the meanwhile, one of my friends suggested I seek help from Medi Journey as he experienced his medical journey very smoothly and was satisfied with it. They have filtered the top 10 doctors as per experience, the success rate of surgery & profile, so it helps us to choose the best treatment in India. "
"For my knee surgery, Medi Journey guided me to BLK Hospital where I received exceptional care. The team's support and the expertise at BLK Hospital exceeded my expectations. Thank you Medi Journey for making my medical journey stress-free. "
"I came from Iraq for my granddaughter's eye surgery in India facilitated by Medi Journey, due to critical cases they advised us to get a second opinion from the different hospitals before going to surgery. Finally, we went to Fortis Escort Hospital, which helped us to get more confidence for diagnosis. Fortis Escort Hospital has the best eye surgeon team with the latest instruments. Thanks to all team members for providing a high-quality treatment in India at an affordable cost. "
"I came for my hair transplant in India, before coming I was so confused about choosing the best clinic and surgeon for me. But thanks to God one of my friends had a hair transplant in India through Medi Journey. He recommended me to go with them. I am completely happy with my experience with them. They were always very fast in their responses to me. the success rate of my hair transplant surgery is 100%."
"Artemis Hospital, suggested by Medi Journey, turned out to be a great choice for my treatment. The personalized assistance and medical care were exceptional. I'm grateful to Medi Journey for guiding me to a hospital that perfectly matched my needs. Highly recommended! "
"I came from Afghanistan for my treatment in India at Jaypee Hospital, Noida. I had a fantastic experience with Medi Journey. Kudos to them for their incredible support during my medical journey. They not only took care of all the logistics but also connected me with a fantastic healthcare team. Efficient, caring, and highly recommended for a hassle-free medical tourism experience."
"I am Adam from Kano, Nigeria, one of my friends from Nigeria was facilitated by Medi Journey, and he recommended us to go with them. I sent my all reports to them and within 48 hours they reverted with 4 options from different hospitals. They helped me to get a Visa letter from the hospital, arrange pick-up from the airport, and book a hotel for me. Their team is very honest and throughout our stay in India they are with us they are caring for us like his family members. BLK Hospital is the best hospital in India with a top surgical oncologist surgeon team, a very advanced OT, and a Radiotherapy department. I wish more success to Medi Journey. "
"Great experience at the Max Hospital for my spine surgery and was successfully done. I thank my neurosurgeon and his entire team. I recommended all of my country's people to Medi Journey for treatment in India, they choose the best hospital, the best doctors, and the best cost for patients."
"I came to India from Dhaka, Bangladesh for my father-in-law's cardiac surgery at Fortis Hospital. I was confused about choosing the best surgeon for him before coming, but their team helped me to choose the best hospital and best cardiac surgeon in India with very good cost and 100% success rate of surgery. I am very happy with the services, really they make my journey so comfortable that make me feel at home. Thanks again and I like people to choose "Medi Journey" as your travel guide. "
"I am Mohammad from Bangladesh came to India for my general health checkup. Medi Journey offers me the complete package including Pick-up from the airport, hotel services, and 24-hour assistance. They guide you to choose the best hospital in India, the best cost of treatment with top-most doctors and give you complete information about hotel booking, and pick-up from the airport before coming to India They have the best team to help. Always choose Medi Journey for your treatment in India."