Top Nephrologists in Indraprastha Apollo Hospital Delhi
 04 February,2026
Read More
04 February,2026
Read More
Enquire now in case of any assistance needed
 18 July,2025
18 July,2025
Chronic Kidney Disease (CKD) in India is often called a silent threat, progressing slowly and quietly until it demands urgent medical intervention. For thousands of individuals in India, the journey with CKD begins not in a hospital, but with subtle signs easily missed: persistent fatigue, swelling in the legs, or uncontrolled blood pressure. By the time these symptoms are recognized, many are already facing decisions about dialysis or transplantation.
Across India, families navigate a complex landscape of medical options, financial hurdles, and emotional strain. While access to care has improved significantly through government programs and policy reforms, the experience of living with CKD still varies greatly between urban and rural regions. From state-run dialysis units to home-based peritoneal care and transplant referrals, the Indian healthcare system is getting better.
This blog explores how India is responding to CKD through early diagnosis, expanding dialysis access, and streamlining pre-transplant care.
Fill up the form and get assured assitance within 24 hrs!
Research suggests that almost 10% of the world population suffers from some level of kidney dysfunction. Contributing factors include hypertension, diabetes, and use of over-the-counter medicines, which are known risk drivers of kidney damage.
Despite the challenges, India has witnessed remarkable success stories that inspire hope. The launch of the Pradhan Mantri National Dialysis Programme (PMNDP) has revolutionized access to dialysis care, particularly for economically disadvantaged populations. Under this program, over 3,000 dialysis centers have been established nationwide, offering free dialysis sessions to eligible patients.
Several states have emerged as models of excellence in CKD management. Tamil Nadu's comprehensive kidney care program has achieved a 40% reduction in CKD-related mortality over the past five years. Similarly, Kerala's community-based screening initiatives have successfully identified early-stage CKD in over 200,000 individuals, allowing for timely intervention and lifestyle modifications.
The integration of technology has also brought positive changes. Telemedicine platforms now connect rural patients with specialist nephrologists in urban centers, breaking down geographical barriers. Mobile health applications help patients track their medication schedules, dietary intake, and vital parameters, empowering them to take an active role in their health journey.
Dialysis treatment in India is becoming increasingly affordable and accessible. Public hospital sessions typically cost around INR 2,500, while private clinics may charge more than INR 5,000 per session. However, government initiatives have made significant strides in reducing this financial burden.
For example, the Delhi government recently deployed an additional 150 dialysis machines across six public hospitals to expand the reach of care. The Central Government Health Scheme (CGHS) and various state health insurance programs now cover the cost of dialysis, making treatment accessible to millions of beneficiaries.
India's healthcare system has embraced innovative approaches to CKD management. The development of indigenous dialysis machines has reduced treatment costs by 30% while maintaining international quality standards. Indian manufacturers, such as Nephroplus and Fresenius Kabi, have established world-class production facilities, making India a hub for affordable dialysis equipment.
Home-based peritoneal dialysis programs have shown exceptional results, with patient satisfaction rates exceeding 85%. These programs not only reduce healthcare costs but also allow patients to maintain their daily routines and family relationships while receiving treatment.
Early diagnosis is still the most powerful intervention. The ICMR and Ministry of Health issued Standard Treatment Workflows recommending eGFR, serum creatinine, blood pressure checks, urinalysis, and avoidance of nephrotoxic drugs in primary care.
Nutritional guidelines include a lower protein intake (0.6–0.8 g/kg/day), a low-sodium salt diet (<5 g/day), and restriction on potassium-rich foods in advanced disease.
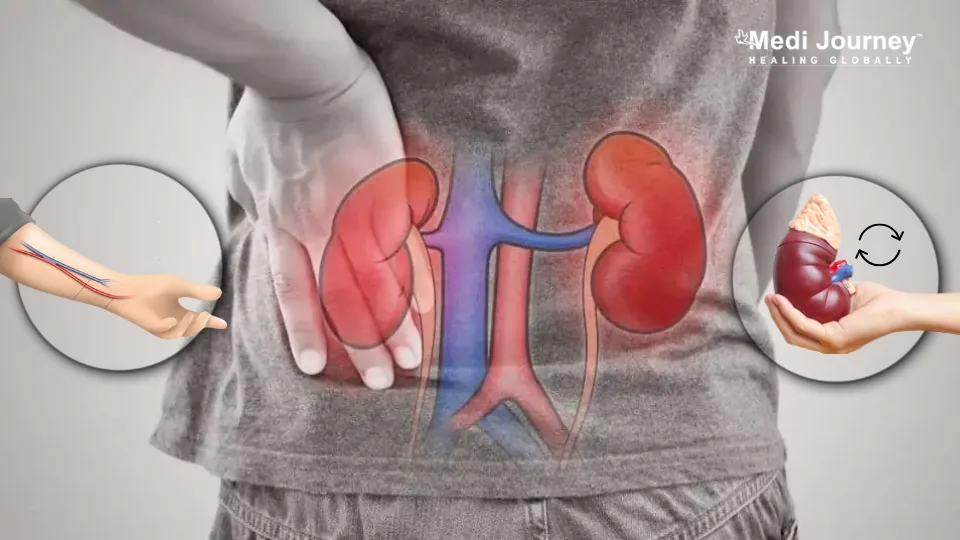
Once patients reach an of less than 30 mL/min, referrals to a nephrologist become critical. In district hospitals, the creation of vascular access (AV fistula or PDa) is a standard procedure. Tertiary centres offer kidney biopsies, imaging, psychological assessments, and discussions on renal replacement therapy (RRT) options.
The graph below outlines how CKD treatment evolves across different stages, offering a clear view of when lifestyle changes, medications, dialysis, or transplant become necessary.

Most ESRD patients (around 94%) undergo haemodialysis, which requires professional staff and machine-intensive setups. While efficient, HD is costly and often concentrated in urban centres, leaving rural populations underserved.
To address this, the government has been promoting peritoneal dialysis (PD)—a home-based alternative that requires less infrastructure and is better suited for remote locations. By the end of 2022, several states had initiated PD programs, exhibiting promising signs of success and cost savings.
Transplant referral is usually suggested once eGFR dips below 30 or symptoms worsen. Pre-transplant setup involves preserving veins for access (usually in the non-dominant arm), conducting a comprehensive workup (including lab tests and imaging), counseling patients and their families, and adhering to legal frameworks outlined in the Transplantation of Human Organs and Tissues Act (1994, amended 2011).
Most transplants still rely on living donors. Equally, financial aid often overlooks long-term postoperative care, meaning patients may struggle to afford ongoing immunosuppressants.
The emergence of patient support groups and non-governmental organizations has created a strong network of hope and resilience. Organizations like the Kidney Warrior Foundation and Amar Gandhi Foundation provide emotional support, financial assistance, and advocacy for CKD patients and their families.
Community-based rehabilitation programs have helped thousands of patients return to productive lives post-treatment. These programs focus on vocational training, psychological counseling, and peer support, ensuring patients with CKD can maintain their dignity and independence.
CKD management in India can be transformed through:
Nephrology care in India requires a connected effort, from early screening and community awareness to home-based dialysis and fair transplant access.
By blending government schemes, digital tools, clinical best practices, and patient-centered care, India could make a meaningful difference in the lives of millions living with CKD.
The future of CKD management in India looks promising, with continued investment in healthcare infrastructure, technological innovations, and patient-centric care models. With collective effort and sustained commitment, India can transform the approach of kidney care, providing hope to millions of patients and their families worldwide.
Answer: Yes, many people with CKD live full and active lives. While the kidneys may not recover from existing damage, the condition doesn't always worsen. Only a small number of people reach advanced stages of the disease. With regular checkups, healthy habits, and the proper treatment, CKD can be managed for years without significant issues.
Answer: Managing CKD means taking care of your overall health. This includes maintaining blood pressure and blood sugar levels within a healthy range, taking prescribed medications on time, working closely with your healthcare team, eating a balanced diet, staying physically active, keeping a healthy weight, and getting sufficient sleep.
Answer: Some small but meaningful changes can help. Quitting smoking, eating a balanced diet, reducing salt intake to less than 6 grams a day (approximately one teaspoon), and staying physically active for at least 150 minutes a week are all recommended. These changes support your kidney health and overall well-being.
Answer: Doctors often use four treatment types to help protect the kidneys:
These help slow down kidney damage, especially in people with diabetes-related kidney issues.
Fill up the form and get assured assitance within 24 hrs!
B.Sc in Media Science from NSHM Knowledge Campus, Kolkata, 2019-2022
Suryani Dutta is an experienced content writer, specializing in healthcare and medical tourism. With a B.Sc. in Media Science from NSHM Knowledge Campus, Kolkata, she creates engaging, accurate, and SEO-friendly content that empowers patients to make info
Director
Kidney Transplant Surgeon, Uro-oncologist, Urologist
Aakash Healthcare Super Speciality Hospital, Dwarka, New Delhi
Dr. Vikas Agarwal is a reputed Urologist and Kidney Transplant Surgeon with an experience of more than 22 years. His expertise lies in a wide range of laparoscopic surgeries, including laparoscopic donor nephrectomy, kidney, prostate, and bladder cancer surgery....
Senior Consultant
Medical Oncologist
Nanavati Super Specialty Hospital, Mumbai
WhatsApp UsSenior Director
Gynecologist and Obstetrician, IVF Specialist
Max Super Speciality Hospital, Shalimar Bagh, New Delhi
WhatsApp UsSenior Director
Gynecologist and Obstetrician, IVF Specialist
Max Smart Super Speciality Hospital, Saket, New Delhi
WhatsApp UsSenior Director
Gynecologist and Obstetrician
Max Smart Super Speciality Hospital, Saket, New Delhi
WhatsApp UsSenior Director
Gynecologist and Obstetrician
Max Smart Super Speciality Hospital, Saket, New Delhi
WhatsApp UsSenior Director
Gynecologist and Obstetrician
Max Smart Super Speciality Hospital, Saket, New Delhi
WhatsApp UsThe Art of Effective Communication
 04 February,2026
Read More
04 February,2026
Read More
 02 February,2026
Read More
02 February,2026
Read More
 27 January,2026
Read More
27 January,2026
Read More
 20 January,2026
Read More
20 January,2026
Read More
 16 January,2026
Read More
16 January,2026
Read More
Trusted by Patients
"I am Asim from Bangladesh and was looking for treatment in India for neuro. I visited many websites to get the complete information regarding the treatment but I was not satisfied as I was getting confused. In the meanwhile, one of my friends suggested I seek help from Medi Journey as he experienced his medical journey very smoothly and was satisfied with it. They have filtered the top 10 doctors as per experience, the success rate of surgery & profile, so it helps us to choose the best treatment in India. "
"For my knee surgery, Medi Journey guided me to BLK Hospital where I received exceptional care. The team's support and the expertise at BLK Hospital exceeded my expectations. Thank you Medi Journey for making my medical journey stress-free. "
"I came from Iraq for my granddaughter's eye surgery in India facilitated by Medi Journey, due to critical cases they advised us to get a second opinion from the different hospitals before going to surgery. Finally, we went to Fortis Escort Hospital, which helped us to get more confidence for diagnosis. Fortis Escort Hospital has the best eye surgeon team with the latest instruments. Thanks to all team members for providing a high-quality treatment in India at an affordable cost. "
"I came for my hair transplant in India, before coming I was so confused about choosing the best clinic and surgeon for me. But thanks to God one of my friends had a hair transplant in India through Medi Journey. He recommended me to go with them. I am completely happy with my experience with them. They were always very fast in their responses to me. the success rate of my hair transplant surgery is 100%."
"Artemis Hospital, suggested by Medi Journey, turned out to be a great choice for my treatment. The personalized assistance and medical care were exceptional. I'm grateful to Medi Journey for guiding me to a hospital that perfectly matched my needs. Highly recommended! "
"I came from Afghanistan for my treatment in India at Jaypee Hospital, Noida. I had a fantastic experience with Medi Journey. Kudos to them for their incredible support during my medical journey. They not only took care of all the logistics but also connected me with a fantastic healthcare team. Efficient, caring, and highly recommended for a hassle-free medical tourism experience."
"I am Adam from Kano, Nigeria, one of my friends from Nigeria was facilitated by Medi Journey, and he recommended us to go with them. I sent my all reports to them and within 48 hours they reverted with 4 options from different hospitals. They helped me to get a Visa letter from the hospital, arrange pick-up from the airport, and book a hotel for me. Their team is very honest and throughout our stay in India they are with us they are caring for us like his family members. BLK Hospital is the best hospital in India with a top surgical oncologist surgeon team, a very advanced OT, and a Radiotherapy department. I wish more success to Medi Journey. "
"Great experience at the Max Hospital for my spine surgery and was successfully done. I thank my neurosurgeon and his entire team. I recommended all of my country's people to Medi Journey for treatment in India, they choose the best hospital, the best doctors, and the best cost for patients."
"I came to India from Dhaka, Bangladesh for my father-in-law's cardiac surgery at Fortis Hospital. I was confused about choosing the best surgeon for him before coming, but their team helped me to choose the best hospital and best cardiac surgeon in India with very good cost and 100% success rate of surgery. I am very happy with the services, really they make my journey so comfortable that make me feel at home. Thanks again and I like people to choose "Medi Journey" as your travel guide. "
"I am Mohammad from Bangladesh came to India for my general health checkup. Medi Journey offers me the complete package including Pick-up from the airport, hotel services, and 24-hour assistance. They guide you to choose the best hospital in India, the best cost of treatment with top-most doctors and give you complete information about hotel booking, and pick-up from the airport before coming to India They have the best team to help. Always choose Medi Journey for your treatment in India."